The U.S. has the highest rate of maternal mortality in the developed world. Yet these deaths of women from causes related to pregnancy or childbirth are almost invisible. When a new or expectant mother dies, her obituary rarely mentions the circumstances. Her identity is shrouded by medical institutions, regulators and state maternal mortality review committees. Her loved ones mourn her loss in private. The lessons to be learned from her death are often lost as well.
The inability, or unwillingness, of states and the federal government to track maternal deaths has been called “an international embarrassment.” To help fill this gap, ProPublica and NPR have spent the last few months searching social media and other sources for mothers who died, trying to understand what happened to them and why. So far, we’ve identified 134 pregnancy- and childbirth-related deaths for 2016 out of an estimated U.S. total of 700 to 900. Together these women form a picture of maternal mortality that is more racially, economically, geographically and medically diverse than many people might expect. Their ages ranged from 16 to 43; their causes of death, from hemorrhage to infection, complications of pre-existing medical conditions, and suicide. We were struck by how many perished in the postpartum period, by the number of heart-related deaths, by the contributing role sometimes played by severe depression and mood disorders — and by the many missed opportunities to save lives.
ProPublica and NPR plan to expand our 2016 photo gallery as we find more women and hear from more families. If you know of someone who died, please tell us here. Meanwhile, we highlight 16 women with portraits of their lives and deaths. Their stories are a reminder of just how much is lost when a mother dies. Examined together, these private tragedies point to a much bigger public health problem, and underscore the potential repercussions for women and families as Republicans in Congress push to revamp the health care system and roll back Medicaid.
January 26
Amanda Rose Kotrba
Amanda Rose Kotrba never got over the frightening birth of her son, back in 2008. Late in her third trimester, she had developed a problem with her placenta — the organ that supplies nutrients to the developing fetus — and lost most of her amniotic fluid, resulting in an emergency Cesarean section. Seven years and a couple of miscarriages later, she was pregnant again. “She was scared,” her mother, Connie Holyfield, said. “She kept telling me that she was scared.”
Amanda was no shrinking violet — “feisty” and “headstrong” is how Connie described her 30-year-old daughter. She worked as a security guard and had a side business cleaning apartments in the Orange Park, Florida, complex where she and her longtime boyfriend lived with their son. She didn’t have private health insurance or a car, but Medicaid covered her maternity care and provided transportation to prenatal appointments; other times, Connie would drive her. Toward the end of her ninth month, Amanda’s visits to the doctor and the emergency room became more frequent. “She started having some bleeding, some back pain and some stomach pain,” Connie said. “She kept telling me she didn’t feel right.” Amanda worried that her placenta was failing again. But the doctors and nurses who examined her always sent her home.
On Sunday, Jan. 24, Amanda was overcome by searing pain; when Connie arrived at the hospital, her daughter was undergoing another emergency C-section. Amanda had suffered a placental abruption — the organ had become detached from the walls of the uterus — and major bleeding. Her newborn daughter had a collapsed lung, and Amanda was so ill she could barely glance at the baby. After a few hours, she seemed to rally. Then, when Connie went to take a photo of the baby to bring back to her room, Amanda texted her: “More blood.” As Connie was signing consent forms for more emergency surgeries, Amanda gasped, “Mom, I’m not gonna make it.” She died 36 hours later, her body so ravaged that, her mother said, “She didn’t even look like the same person.”
February 24
Emily Cook Dyches
Thirty-nine-year-old Emily Cook Dyches of Salem, Utah, “was the mom who learned your kids’ names and asked about them when she saw you,” her husband Eric wrote last year. “She was the neighbor with the untidy house and smiling children. She was the mom who worried about not measuring up, but always put her best foot forward.” Emily and Eric met in third grade and married while attending Brigham Young University in 1998. She taught elementary school for a few years and worked as a piano instructor and photographer, but her most important job, she believed, was raising her kids — teaching them “not only practical life lessons, but more importantly eternal lessons, centered on how one can progressively become more like the Savior in word and deed,” as her obituary put it.
After she nearly died delivering her fifth baby, Trey, in March 2015, she recovered physically, but emotionally she was never the same. When breastfeeding proved difficult, “her anxiety about Trey’s health went through the roof,” Eric said. “She was worried about him developing and growing and surviving.” She began having panic attacks. “I’ve heard it described that it’s like you’re in a jetliner and you feel like the jetliner’s going down,” Eric said. The attacks were so bad he took her to the emergency room a couple of times, but the medical system “is just not equipped to handle that type of emergency.”
Antidepressants helped, and Emily’s condition seemed to stabilize for a time. But in retrospect, Eric said, “she wasn’t fully there, even though I thought we were functioning at a pretty good level.” When Trey was about nine months old, “she came to me and essentially just said, ‘It’s coming back.’” Emily agreed to check into a psychiatric hospital and stayed for 11 nights. (As she and Eric later learned, their insurance wouldn’t have covered visits to an outpatient facility anyway.) The experience was “very similar to incarceration,” Eric said. Emily couldn’t even wear an underwire bra, for fear she might use the wire to harm herself. Still, she got better, and the first couple of weeks after she was discharged felt to Eric like “a second honeymoon.” Then she regressed. On Feb. 24, after spending the day with her parents, she had a panic attack during a car ride. Her father pulled the car to the side of the freeway to console her, but before he could stop her, she opened the door and ran into oncoming traffic.
According to researchers in Georgia, Michigan and other states, mental health disorders have become a leading contributor to maternal deaths among white women in the months after childbirth. Eric doesn’t believe his wife was trying to harm herself. “She was disoriented. She wasn’t sure where she was going.” He does believe she needed more help than her family and community could provide. A few weeks after her death, he started a foundation in her honor, The Emily Effect, to help other women suffering from perinatal mood disorders, with a special focus on improving maternal care in Utah.
March 2
Brittany Haefke
At 23, Brittany Haefke was a stay-at-home single mom with a 6-year-old daughter and a 3-year-old son. She’d struggled with depression and drugs over the years, chronicling her ups and downs in her diaries, according to her mother, Deneen Haefke. But her kids helped keep her grounded. Nothing made her happier than playing ball with them or teaching them to ride their bikes. “You could just see the joy in her face,” Deneen said. “You couldn’t rip her away from them.”
Just hours after the birth of her third child, Cole, on Feb. 11, 2016, Brittany had so much trouble breathing that doctors put her on oxygen. She was so swollen, Deneen said, “she still kind of looked like she was pregnant.” The hospital staff ran some tests, but when Brittany heard the results she was so upset that she checked out and refused to tell her mother what the doctors had said. Back at the home the family shared in Floral City, Florida, Brittany withdrew into herself. “She did not even try to bond with [the baby],” Deneen said. Her swelling grew worse, and she started having chest pains. “I asked her every day, ‘Please let me take you to the doctor.’ She would refuse.” One morning, Brittany called her mother from a friend’s house: She was on her way to the hospital and didn’t think she’d be coming home. She died a few hours later from pregnancy-induced heart failure — the diagnosis, Deneen believes, that doctors had given her three weeks before. The condition is often treatable, but recovery can be long and uncertain, and Brittany’s Medicaid benefits were set to expire a couple of months after she delivered.
Her final journal entries reflected that she was tired of fighting. “I think she gave up on life,” Deneen said. Her mother buried the diaries with her.
April 8
Marqwetta Johnson
Marqwetta Johnson of Tulsa, Oklahoma, had no idea when she collapsed that she was six weeks pregnant with twins. At 42, she had seven children, including a daughter with a learning disability, a son with autism, and twin 3-year-olds. The family was poor, but Marqwetta was patient and loving, said her eldest, 23-year-old Jamal. “She would tell me, ‘Whatever you decide to do, do the best you can at it.’” With his mother’s encouragement, he earned his undergraduate degree at Oral Roberts University in 2015, then headed to China to study international relations and Mandarin. He called her from there on April 7, 2016. “She was fine, laughing and telling me to make sure I did my Chinese homework.”
The next morning, Marqwetta complained of pain in her abdomen and began to bleed. Rushed to the hospital, she was diagnosed with an ectopic pregnancy. One or more fertilized eggs had implanted in her fallopian tube instead of her uterus and burst, leading to hemorrhage and cardiac arrest. Marqwetta was older and overweight, traits associated with higher rates of pregnancy complications. Another risk factor was poverty. “She did not go to the doctor very often,” Jamal said. “I think people have a fear of going to see the doctor because of the cost associated with it. The uncertainty and the fear of, ‘Well if there is something wrong, it’s gonna be more expensive for me to try to fix what’s wrong.’” His mother’s sudden death left his younger siblings “like sheep without the shepherd,” he said. “That’s when it was my turn to stand up and say, ‘No, everything’s going to be okay.’” Jamal flew back to Tulsa and, fearing that the state would put his brothers and sister into foster care, launched a GoFundMe campaign to help him gain custody of them. He raised almost $20,000, enough to rent a house, hire a lawyer, and keep his family intact. He also got married and is expecting a child of his own. If he could see his mother one last time, he said, “I would tell her that all of her babies are okay. Including me.”
April 13
Kira Dixon Johnson
The YouTube video commemorating Kira Dixon Johnson’s life shows a vibrant woman who seemed to be in perpetual motion — racing cars and jet skis, piloting a plane, splashing in the ocean with her firstborn, Charles, in her arms. She spoke five languages and started a chain of English-language schools in China in the 2000s, then worked in the restaurant business in her native Atlanta. There she fell in love with Charles Johnson IV, from a prominent family of educators and civil rights lawyers. (His mother, the one-time TV judge Glenda Hatchett, represented the family of Philando Castile, gunned down by a police officer in Minnesota last July.) “She was literally the closest thing I’ve ever met to Wonder Woman,” her husband said. “She was superhuman to me.”
Kira was six months pregnant with her second son, Langston, when the couple moved to Los Angeles to pursue various business projects. She had delivered her first child by emergency C-section, and, hoping to avoid another trauma, she chose doctors affiliated with one of the city’s premier hospitals, Cedars-Sinai Medical Center. The delivery “was supposed to be a walk in the park,” Charles said. But soon after her scheduled C-section, Kira, 39, began to hemorrhage. Obstetric bleeding is one of the most common causes of maternal deaths in the U.S.; 70 percent of such deaths are preventable, researchers in California have found. In Kira’s case, her family contends, the medical team delayed treatment too long. Her abdominal cavity filled with blood and she died 12 hours after giving birth.
Charles sued the hospital and doctors this past spring in Los Angeles County Superior Court. The family hopes that the case will help spotlight the issue of maternal mortality among blacks, who die at a much higher rate than other women. “I owe it to my wife,” he said. “I owe it to my sons.” The hospital and doctors denied the allegations in court papers, contending that any negligence on their part was “not a substantial factor” in Kira’s death. In a statement, the hospital commended Kira’s family for “demonstrating important leadership in raising awareness of preventable maternal deaths,” adding: “[W]e thoroughly investigate any situation where there are concerns about a patient’s medical care. Based on our findings, we make any changes that are needed so that we can continue to provide the highest quality care to our patients.”
May 15
Amy Bartlett
Amy Bartlett was the Yellowstone National Park spokeswoman who went on the news to explain why it was a stupid idea to take selfies with a giant bison or why scientists were sure the mega-volcano under the park was not about to blow. Yellowstone wasn’t just her job, it was her life: She met and married her husband, Jerry, there, made her home on the park’s Montana border, and named her kids Jackson (for the Wyoming resort town to the south of the park), Hayden (for the valley) and Ella Faith (for the geyser). Ella was born May 7, 2016.
At 41, Amy was thrilled to finally have a daughter. But a week after going home, while Jerry was putting the boys to bed, Amy suddenly began feeling strange — pain in her neck and jaw, a galloping heartbeat, extremely high blood-pressure readings on her home monitor. First she called her mother, then a friend who was coordinator of emergency medical services for the park. They told her the same thing: Her symptoms sounded like a heart attack. She needed to get to the hospital right away. Amy and Jerry both had EMS training, so they recognized the symptoms, too. But Amy was in excellent health, it was the middle of the night, and they lived more than an hour away from the medical center in Bozeman — a long way to go for a false alarm.
Amy opted to phone one more person, an on-call doctor at the hospital who suggested she rest a few minutes, then re-measure her blood pressure. As she lay down and began nursing, Jerry snuggled into bed beside her. At first, he thought she had fallen asleep; then he realized she had stopped breathing. An autopsy revealed a spontaneous coronary artery dissection, or SCAD, in which one of the main arteries to the heart suddenly splits. Once mistakenly thought to be quite rare, SCAD is now recognized as one of a series of heart conditions that may be triggered by pregnancy hormones, even in women who are otherwise healthy. The condition isn’t preventable, but if he and Amy had ever heard of it, Jerry said, they might have been able to save her life. “Neither of us wanted to believe this could be happening to her,” he said.
May 17
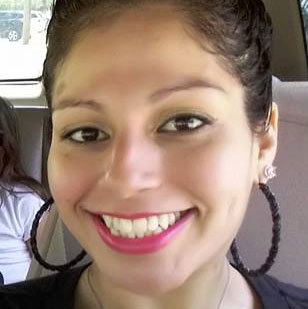
Krystine Toledo-Gonzalez
Krystine Toledo-Gonzalez loved to dance and hang out with friends — “things I would never, ever do if it wasn’t for her,” said her husband, Luis. “She was always pushing me to do more. We pushed each other.” They met in Miami in the mid-2000s and moved to Georgia a few years later to work and raise a family. He was a manager at Costco Wholesale; she was a part-time post-operative nurse in the Northside Hospital system and took care of their three kids, ages 2 to 16.
Krystine had given birth to her youngest child by emergency C-section, something she didn’t want to go through again. When she found out she was expecting another baby, she was determined to have a VBAC (vaginal birth after cesarean). Many ob/gyns and hospitals refuse to perform VBACs because of concerns that the uterus could rupture, so she had to go to Northside’s main hospital in Atlanta, which delivers 15,000 babies a year — more than any other medical center in the U.S.
Krystine had a slight fever but the delivery went fine. Then doctors discovered that she had developed a cold sore, so they decided to put her in isolation for a few days, Luis said. When she began complaining of pain in her abdomen, the first assumption was that she was having indigestion — gas trapped in her gut because she wasn’t able to walk around as much as she wanted. The pain worsened and her condition deteriorated. By the time she was diagnosed with a staph infection, Luis said, doctors couldn’t save her. She died at the age of 30, six days after her daughter was born.
“Northside Hospital shares in the loss of Krystine Toledo-Gonzalez,” the hospital said in a statement. “Privacy laws prevent us from providing any comments or additional information.”
May 27
Lynn Aguibitin Welker
Lynn Aguibitin Welker didn’t realize she was pregnant until her fifth month for a very good reason; she’d had her fallopian tubes tied after the birth of her second child. At 38, she worked in the preschool at Mission College in Santa Clara, Calif. “She was a great teacher, passionate about doing that,” said her husband, Eric, who met her in high school in the early 1990s when they were both in Junior ROTC. At school and at home, she was constantly making music and art. She wanted her daughter, 8-year-old Jordan, and son, Noah, 5, “to think crazy, whimsical ideas,” Eric said. “She was very much about raising kids who can see the potential in things.”
Finding out she was pregnant again “was a nice surprise,” he said. Then, two weeks later, an ultrasound revealed that the baby had hypoplastic left heart syndrome, a severe congenital defect that would require open-heart surgery soon after birth. Lynn “started to blame herself a little bit,” Eric said. She had chronic high blood pressure, and though doctors tried to reassure her, she worried that her anti-hypertensive medication might have hurt the baby.
For the next few months, she and her physicians did what they could to give the baby the best chance at a healthy life. On May 27, 2016, Lynn had a C-section at the University of California, San Francisco Medical Center and neonatal specialists whisked away the fragile newborn, Savannah Angel. Lynn seemed fine. Then she crashed, and doctors couldn’t bring her back.
According to the autopsy, she had major blockages in her arteries that had gone unnoticed for years, leading to a massive coronary. The news was better for Savannah. After two surgeries, she’s strong and healthy, beginning to crawl and babbling her first words — “Da-da” and “Ma-ma-ma-ma.” “She’s doing great,” Eric said. “It’s been a good example of resilience for me to see.”
June 15
Laura Lenss
Laura Lenss, a 38-year-old architect in Seattle, “was like a Renaissance woman,” her older sister Kristina Lenss said. “She was absolutely an expert at every single thing she did, whether it was architecture or building furniture or cooking or illustrating or making clothes or making movies. You name it.” Motherhood was Laura’s most absorbing project; she had one son, 3-year-old Henry, and was eagerly awaiting the arrival of his brother, whom she planned to name Wally. At her final prenatal appointment, her doctor suggested an induction that day. Laura texted Kristina that she was in the hospital eating a salad and then she would have the baby.
Labor went extremely quickly — less than an hour, Kristina said. Laura suffered a third-degree tear in her perineum, or vaginal area, but told her sister she wasn’t worried; the same thing had happened with Henry. Back home with the baby after one night in the hospital, “she was so excited,” Kristina said. “She said, ‘I’m just so in love. He’s perfect. He’s beautiful.’”
Soon, though, Laura was complaining about severe pain in her neck and shoulders. In a photo taken at Wally’s first pediatric appointment on June 14, she looked swollen and exhausted. That night, Laura was so self-conscious about her bloated appearance that she didn’t want to Facetime with her family. She made an appointment with her doctor for the next morning, but when her parents came to pick her up, they took one look and called 911. She died on the operating table a few hours later from complications of a strep A infection that began in her perineal wound.
“We’ve been crying ever since,” Kristina said. “We cry every day.”
June 30
Larissa Icemen
At 25, Larissa Icemen was sweet but shy — the result, her mother-in-law Roberta Russette thought, of growing up in rough circumstances in Minneapolis’s Native American community. At big gatherings, she often kept to herself, and at home, she focused on her kids. She was pregnant with her fourth child.
On the morning of Feb. 6, 2016, in her 38th week, her husband Landen took her to University of Minnesota Masonic Children’s Hospital for what they expected would be another smooth delivery. Soon after they arrived, Larissa began vomiting and went into cardiac arrest. Doctors delivered her healthy son by emergency C-section, then rushed her to another hospital, where she underwent surgery for an amniotic fluid embolism, a rare complication believed to occur when amniotic fluid or other fetal material — sometimes as tiny as a fingernail or a hair — enters the mother’s bloodstream, triggering a massive allergic-like response.
The embolism caused Larissa’s heart to stop several times, depriving her brain of oxygen. When her condition stabilized, she was transferred to a nursing home. She couldn’t walk or talk, but she responded to her caregivers and family enough to give them hope. “She would have these really fighting moments… these bright spots,” Roberta said. “Then she would slip. All of a sudden she would get an infection out of nowhere.” She languished for almost five months. “We didn’t speak about it,” Roberta said. “We just knew she wasn’t going to fight anymore.”
July 13
Amanda Eva Garcia
Twenty-six-year-old Amanda Eva Garcia lived in Texas, where maternal deaths have increased sharply in recent years. One of 16 siblings, “she came from a really hard life,” said Zak Tiemann, her boyfriend since 2011. She was sweet-natured and excitable, with a raucous laugh that burst out of nowhere — “little things put a big smile on her face.” She especially doted on her 9-year-old daughter, June, and their 2-year-old, Zoey. “Her mom abilities were so good,” Zak said. “She was the best mom I’ve ever seen.”
Amanda didn’t earn enough in her assembly-line job making foam food containers to afford insurance, so like more than half of women who give birth in Texas, she got her care through Medicaid. After delivering her third daughter, Zayleeana, by C-section on July 5, 2016, she and the kids went to stay with Zak’s mom while he picked up work in San Antonio, 35 miles away.
A couple of days after leaving the hospital, Amanda’s stomach started to ache. She lost her appetite: “She wasn’t eating her food. She was just throwing it in the trash,” Zak said. She turned pale and complained of feeling hot even though, to Zak’s touch, “her body felt real, real cold.” Eight days after giving birth, she could no longer stand up. An ambulance took her to Guadalupe Regional Medical Center, where doctors told Zak that her organs were failing. She passed away a couple of hours later.
August 14
Sheriah Freitas
Sheriah Freitas met her husband Deitton, a soldier in the U.S. Army, at a Walgreens in Hawaii, where she was working in the cosmetics department. He loved her beautiful eyes — “they’re like blue and green and gray with brown in them” — and her big personality. “She was fierce. She was strong-minded and confident.” Pregnant with her first child at 25, she appeared to be doing exceptionally well. “We went to every appointment, every ultrasound, everything was perfect,” Deitton said. Still, he couldn’t help fretting, especially after they received transfer orders to Fort Benning, Georgia, thousands of miles from their families. “I just worried about my wife all the time.”
Sheriah went into labor three weeks early, on Aug. 13, 2016, but the couple was more excited than concerned. “We were making jokes all day,” Deitton said.
Then the mood shifted. Doctors said labor wasn’t progressing properly and that Sheriah needed a C-section. After the surgery, she held baby Luther — they’d settled on his name while she was in labor — for a few minutes. Then she began to bleed uncontrollably.
Sheriah had developed an amniotic fluid embolism. Doctors don’t know how to predict or prevent them; up to 80 percent of mothers who develop amniotic fluid embolisms die. Soon Sheriah went into cardiac arrest; Deitton held her hand and prayed while doctors worked frantically to revive her. He was still clutching her hand when she died.
September 4
Audrey Lockett LaBranche
Audrey Lockett LaBranche was a dynamo with a huge smile, a constantly changing assortment of colorful hairstyles, and vast reserves of energy, ambition and faith. She was the founder and proprietor of LaBranche’s Childcare Center, in Chicago Heights, Illinois, which provided care for 60 kids at a time, from babies in diapers to latch-key tweens, as well as support for their harried parents.
Under the name Audrey Cher, she had a side career as a Christian neo-soul/funk singer and songwriter and released her debut solo album, “The Intro,” last year. Her busy household included her husband of 21 years, a teenage son and daughter and 7-year-old twins. “I’m overwhelmed with Love & thanks,” she posted on Facebook last summer, pregnant with her fifth child. “I’m thankful for my life’s journey and I would not trade anything for the path I walked to get to where I am today.”
Her final pregnancy felt especially improbable. In 2015, Audrey had developed multiple blood clots that traveled to her lungs and nearly killed her. After months of medication and rest, she’d made a complete recovery. Then, as she announced on Facebook in January 2016, “God decided to surprise us.” The pregnancy was anything but easy. Audrey was 39, overweight and had thyroid disease. She was on blood thinners to prevent clots, but she experienced frequent Braxton Hicks contractions (uterine contractions that mimic labor) that made her uncomfortable and worried that the clots might be coming back. Late in the pregnancy, after a falling out with her longtime ob/gyn, she switched to a new doctor. “It was stressful to have to go under the care of someone who did not know her history,” her mother, Kathleen Lockett, said. But after that, things seemed to proceed smoothly, and baby Mathias was born by C-section in late August 2016, weighing eight pounds.
A couple of days after returning home, Audrey started complaining of a headache and problems with her C-section incision. At the local hospital, she was told that her sinuses were probably acting up, Kathleen said. The headache grew worse, and on Friday, Sept. 2, Audrey’s husband Marcus reported on Facebook that she had been rushed to a trauma center in Chicago: “My wife has suffered severe hemorrhaging in her brain that has left her in a lifeless state.” He was determined to stay hopeful. “Satan is a confirmed fool if he thinks this will shake my faith!”
But on Sept. 4, he acknowledged that Audrey still hadn’t shown any signs of improvement. She died that afternoon.
September 6
Marlene Dominguez-Hicks
Marlene Dominguez-Hicks, 33, was the pride of her Filipino-immigrant parents — valedictorian of her high school class, B.A. from Stanford, M.D. from Meharry Medical College in Nashville.
She and her family — husband Alex, daughters Alyssa and Alana — were living in Houston, where she was in a radiology program at the University of Texas Health Science Center and looking forward to the birth of Alex Jr. Two weeks before the baby was due, she could still run up the stairs of her town house, declaring to her husband, “I feel great.” In her maternity photos taken around the same time, she wore a long white dress, a crown of flowers, and a radiant glow.
She spent Labor Day at the park and the zoo with her husband and kids. Alex urged Marlene, “Slow down if you need to,” but she insisted she was fine. The next day, she made her rounds as usual — she figured she might as well work up to the end, since her job was conveniently located in the hospital where she planned to give birth. After dinner, the girls were in bed and Alex was downstairs when he heard what sounded like books falling off a shelf. He found Marlene lying on the bathroom floor, unconscious, blood trickling from her mouth.
Paramedics did their best to revive her, but by the time they reached the hospital, she was gone. Doctors couldn’t save the baby, either — he’d been without oxygen too long. The diagnosis was peripartum cardiomyopathy, a type of heart failure that is induced by pregnancy and can strike from the middle of the second trimester into the postpartum period. It is treatable, but the symptoms — fatigue, swelling, shortness of breath — mimic the normal discomforts of pregnancy and so are often ignored. Once considered quite uncommon, peripartum cardiomyopathy is now estimated to cause about 11 percent of maternal deaths and can have a genetic component. That weighs on Alex’s mind. “When I take the girls to the doctor, I’m always going to ask him or her to check their hearts.”
November 18
Joonyper Light
Joonyper Light was many things — a punk rocker, a college student, a jewelry crafter, a budding businesswoman. She was also a 21-year-old heroin addict with a history of bipolar disorder and depression who was trying hard to change her life.
When she found out she was pregnant, “she got even more adamant” about beating her addiction, and entered a drug treatment program, her fiancé Matt Stock said. But the emotional ups and downs of pregnancy “led to even more of a struggle.” Getting clean in Springfield, Missouri, meant starting over with a whole new group of friends. “She didn’t have too many support systems. She felt alone. Felt bad about me being really her only true support system and putting everything on me.” As difficult as the prenatal period was, Matt said, Joonyper was “terrified of postpartum. She would always tell me, ‘I don’t know how I’m going to deal with this. I’m scared of how I’m going to be during that phase.’”
Their son Monte, born in September 2016, “lit up her life,” Matt said. Still, with Matt working full-time installing solar panels, “there was just not a whole lot of time for her to get to her rehab,” he said. Meanwhile, she worried about taking medications like antidepressants that would get in her breast milk. “She would act fine on the outside but be hurting on the inside.”
The stress and depression became “just too much for her to handle,” he said. Matt came home one night in November to find Joonyper on the bathroom floor, dead of an overdose. She wasn’t unique; maternal mortality review committees in Texas, Colorado and Philadelphia have found that overdoses linked to mood disorders make up an increasing number of maternal deaths. “This was a relapse. This was not an ongoing thing,” Matt wrote on Facebook a couple of days later. Also: “I need help. I really don’t know how to deal with this.”
December 1
Christen Vogel
Christen Vogel, 21, and her mother, Pamela Gore, were as close as some sisters. They lived two hours apart in North Carolina, but they talked several times a day, and Pam regularly drove to Camp Lejeune, where Christen’s husband was a Marine, to attend her daughter’s prenatal appointments. “I was looking forward to being “not a ‘grandma’ but a ‘Pamma,’” Pam said.
The only shadow of a problem emerged in Christen’s 38th week. She texted her mom to say she didn’t want to come home for her maternity photo shoot because she was afraid she might go into premature labor. She told her husband she had a headache, and when he urged her to see a doctor, she said she would try taking some medicine first. On the night of Nov. 30, Christen got out of bed and decided to take a bath. “That was her soothing measure,” Pam said. “If she had a headache, she’d get in the bath. If she had a stomach ache, she’d get in the bath.” When her husband woke up around 5:00 the next morning, he found her unresponsive in the tub. Neither she nor the baby survived.
The question no one seemed able to answer was why. Her heart and other organs were normal, an autopsy showed. The only substances in her bloodstream were caffeine and acetaminophen. The final death certificate listed the cause of death as “undetermined.”
The lack of finality was devastating for Pam, who started a GoFundMe campaign this past April to pay for an independent pathologist to review the records. “I have two other daughters who have hopes of having families in their future,” she wrote. “If this was caused from something that we could have prevented, I need to know.” Donors eventually contributed more than $3,300, but she’s still looking for a pathologist willing to take the case.
-

Tanisha Malloy
- Chesapeake, VA
- Died:
- Age: 33
- Read the obituary
-
Jeneva Beiler
- Lancaster, PA
- Died:
- Age: 29
- Read the obituary
-

Briahna Gerloff
- Pottstown, PA
- Died:
- Age: 18
- Read the obituary
-

Amanda Rose Kotrba
- Orange Park, FL
- Died:
- Age: 30
- Read the obituary
- Read her story
-
Renee Nichole Saylor
- Buffalo, NY
- Died:
- Age: http://buffalonews.com/2016/02/03/renee-nichole-saylor/
-

Cassia Rott
- Clay Center, KS
- Died:
- Age: 36
- Read the obituary
-
Amanda Nichole Little
- Elizabethtown, KY
- Died:
- Age: 28
- Read the obituary
-

Megan Rebecca Seney
- Newport News, VA
- Died:
- Age: 31
- Read the obituary
-

Emily Cook Dyches
- Salem, UT
- Died:
- Age: 39
- Read the obituary
- Read her story
-
Shanta Waller
- Spotsylvania, VA
- Died:
- Read the obituary
-

Brittany Renee Haefke
- Floral City, FL
- Died:
- Age: 23
- Read the obituary
- Read her story
-
Allison Bree Senser
- Columbus, OH
- Died:
- Age: 35
- Read the obituary
-
Jennifer Lynne Knarr
- Bozeman, MT
- Died:
- Age: 34
- Read the obituary
-
Stephanie Lauren Stills
- Oklahoma City, OK
- Died:
- Age: 22
- Read the obituary
-
Ashley Renée MacArther (Raine) Porter
- Lake Jackson, TX
- Died:
- Age: 24
-
Tiffany Lynn Miller
- Laconia, IN
- Died:
- Age: 25
- Read the obituary
-

Domaniek Shepherd
- Dallas, TX
- Died:
- Age: 38
- Read the obituary
-
Ashley Nicole Melton
- Port Wentworth, GA
- Died:
- Age: 27
- Read the obituary
-

Becca Barber Meissner
- Manitowoc, WI
- Died:
- Age: 26
- Read the obituary
-
Rodshecka E. Piggie
- Memphis, TN
- Died:
- Age: 22
- Read the obituary
-

Marqwetta Johnson
- Muskogee, OK
- Died:
- Age: 42
- Read the obituary
- Read her story
-
Hailey Abigail Senior
- New Braunfels, TX
- Died:
- Age: 20
-

Julia Duvall
- Oakland, CA
- Died:
- Age: 29
- Read the obituary
-

Ashlie Lynn Eddy Garcia
- Oklahoma City, OK
- Died:
- Age: 25
- Read the obituary
-
Julia Price Chester
- Florence, AL
- Died:
- Age: 28
- Read the obituary
-

Kira Dixon Johnson
- Los Angeles, CA
- Died:
- Age: 39
- Read the obituary
- Read her story
-
Kimberly LaBar
- East Stroudsburg, NC
- Died:
- Age: 27
- Read the obituary
-
Jamie Shreiner
- Payson, AZ
- Died:
- Age: 33
- Read the obituary
-

Brittany Fleenor
- Williamsburg, KY
- Died:
- Age: 29
- Read the obituary
-
Kerrie Jones Fessler
- Paso Robles, CA
- Died:
-

Elizabeth (Liz) Fraga
- Milford, MA
- Died:
- Age: 26
- Read the obituary
-
Sheree Boyer
- Mobile, AL
- Died:
- Age: 27
- Read the obituary
-

Courtenay McVey
- Florence, AZ
- Died:
-

Natasha Angie
- Las Vegas, NV
- Died:
- Age: 28
-

Amy Bartlett
- Corwin Springs, MT
- Died:
- Age: 41
- Read the obituary
- Read her story
-

Krystine Toledo-Gonzalez
- Sugar Hill, GA
- Died:
- Age: 30
- Read the obituary
- Read her story
-
Dinelle Tynisha Constantine
- Frederick, MD
- Died:
- Age: 33
- Read the obituary
-

Lynn Aguibitin Welker
- San Jose, CA
- Died:
- Age: 38
- Read the obituary
- Read her story
-

Megan Michelle McKee
- Catonsville, MD
- Died:
- Age: 24
- Read the obituary
-
Mercedes Rivera
- Brooklyn, NY
- Died:
- Age: 16
- Read the obituary
-
Melissa Temsook Knott
- Metairie, LA
- Died:
- Age: 34
- Read the obituary
-

Paula Nicola (Nikki) Shoemake-Patterson
- Starkville, MS
- Died:
- Age: 40
- Read the obituary
-

Brandi Beaujon Logsdon
- Johnstown, PA
- Died:
- Age: 25
- Read the obituary
-
Staci Kelly Ness Mann
- Blue Anchor, NJ
- Died:
- Age: 39
- Read the obituary
-
Erica Patterson
- Chicago, IL
- Died:
-

Evelyn Mae Power Rethford
- Kennewick, WA
- Died:
- Read the obituary
-
Tammy Annette Norman Hogan
- Wortham, TX
- Died:
- Age: 24
- Read the obituary
-

Laura Lenss
- Seattle, WA
- Died:
- Age: 38
- Read the obituary
- Read her story
-

Traci Burnley Chocol
- Denver, CO
- Died:
- Age: 49
- Read the obituary
-
LaToya Machon Jones
- Pflugerville, TX
- Died:
- Age: 30
- Read the obituary
-
Felicia Lofty
- Whitwell, TN
- Died:
- Age: 22
- Read the obituary
-

Allison Parker Goldstein
- Richmond, VA
- Died:
- Read the obituary
-
Sadie Lynn Cole Palma
- South Portland, ME
- Died:
- Age: 20
- Read the obituary
-

Larissa Rochelle Icemen
- Minneapolis, MN
- Died:
- Age: 25
- Read her story
-
Shelly Susanne Wolf Posivenko
- Carrollton, GA
- Died:
- Age: 38
- Read the obituary
-
Selah Boyer
- Tucson, AZ
- Died:
- Age: 33
- Read the obituary
-
Cree Brianne Erwin
- Battle Creek, MI
- Died:
- Age: 24
- Read the obituary
-
Tierra Hughes
- Roanoke, VA
- Died:
- Age: 25
- Read the obituary
-

Michelle Lee Sullivan
- Rogers, MN
- Died:
- Age: 30
- Read the obituary
-
Erin Michelle Avery
- Garner, NC
- Died:
- Age: 31
- Read the obituary
-

Chaphley Ornevil Jacques
- York, PA
- Died:
- Age: 41
- Read the obituary
-
Amanda Eva Garcia
- Seguin, TX
- Died:
- Age: 26
- Read her story
-
Gabriela Rojas
- Napa, CA
- Died:
- Age: 27
- Read the obituary
-

Jessica Faumui-Masalosalo
- Anchorage, AK
- Died:
- Age: 25
- Read the obituary
-

Joy Gray Barbat Rusin
- San Diego, CA
- Died:
- Age: 31
- Read the obituary
-

Meagan Duarte
- Northampton, PA
- Died:
- Age: 29
- Read the obituary
-
Khanita Moore-Gordon
- Omaha, NE
- Died:
- Age: 29
- Read the obituary
-
LaMeisha Nichole Haynes
- Folsom, LA
- Died:
- Age: 28
- Read the obituary
-
Amanda (Mandy) Keefer
- Kissimmee, FL
- Died:
- Age: 28
- Read the obituary
-

Deanna Gioia
- Staten Island, NY
- Died:
- Age: 35
- Read the obituary
-

Amy Lam Wai Chi
- New York City, NY
- Died:
- Age: 34
- Read the obituary
-
Melissa Allen
- Tyngsboro, MA
- Died:
- Age: 31
- Read the obituary
-
Sonia Jimenez
- Hughson, CA
- Died:
- Age: 36
- Read the obituary
-
Kylie Joy Hendress
- Brookston, IN
- Died:
- Read the obituary
-

Sheriah Oshiro-Directo Freitas
- Ft. Benning, GA
- Died:
- Age: 25
- Read her story
-

Stacy Ann Gottwaldt
- Coon Rapids, MN
- Died:
- Age: 41
- Read the obituary
-
Gina Decena
- Twain Harte, CA
- Died:
- Age: 39
- Read the obituary
-
Steaphanie Gayle Boswell Shoulars
- Lucama, NC
- Died:
- Age: 24
- Read the obituary
-
Amy McKillip Hines
- Clovis, NM
- Died:
- Age: 33
- Read the obituary
-
Rheanna Denise Buxton
- Douglasville, GA
- Died:
- Age: 27
- Read the obituary
-

Carrie Million Naas
- Chesapeake, VA
- Died:
- Age: 39
- Read the obituary
-
Dahlia Salinas Tatman
- San Diego, CA
- Died:
- Age: 39
- Read the obituary
-
Heather Mills
- Turlock, CA
- Died:
- Age: 31
- Read the obituary
-

Audrey (Cher) Lockett LaBranche
- Crete, IL
- Died:
- Age: 39
- Read her story
-

Cara Cuevas
- Ulster Park, NY
- Died:
- Age: 30
- Read the obituary
-

Marlene Dominguez-Hicks
- Houston, TX
- Died:
- Age: 33
- Read the obituary
- Read her story
-
Tasneshia Rodgers
- Atlanta, GA
- Died:
- Age: 40
- Read the obituary
-
Sandra Trujillo-Corral
- Victorville, CA
- Died:
- Age: 40
- Read the obituary
-
Kimberly Lynn Hamblen
- Grand Junction, CO
- Died:
-
Brooke Sevier
- LaMesa, CA
- Died:
- Age: 30
- Read the obituary
-

Kalee Diane Joy Barton
- Lubbock, TX
- Died:
- Age: 29
- Read the obituary
-
Ashley Nicole Heaney-Butler
- Bayville, NJ
- Died:
- Age: 31
- Read the obituary
-
Kimesha (Kim) Simpson
- Baldwin, NY
- Died:
- Age: 37
- Read the obituary
-

Heather Ruggles
- Pooler, GA
- Died:
- Age: 28
- Read the obituary
-

Heidi Rufi Grice
- Plano, TX
- Died:
- Age: 35
- Read the obituary
-
Amanda Ireland Ward
- Greensboro, NC
- Died:
- Age: 33
- Read the obituary
-

Marilyn Marjorie Desire (Shorty) Charles-Havlik
- Irving, TX
- Died:
- Age: 23
- Read the obituary
-
Blake Titsworth
- Muskogee, OK
- Died:
- Age: 23
- Read the obituary
-
Sarah Louise Lambert
- Lyons, OR
- Died:
- Age: 29
- Read the obituary
-
Christine Bates Madrid
- Las Cruces, NM
- Died:
- Age: 27
- Read the obituary
-
Sonia Cardoso-DaSilva
- Keansburg, NJ
- Died:
- Age: 41
- Read the obituary
-
Tiera Gillespie
- Belleville, IL
- Died:
- Age: 19
- Read the obituary
-
Latisha Fruhauf
- Milbrook, AL
- Died:
- Age: 41
- Read the obituary
-

Nivia Lashaundra McIntosh
- Jacksonville, FL
- Died:
- Age: 36
- Read the obituary
-
Denise Moore
- Fuquay-Varina, NC
- Died:
- Age: 39
- Read the obituary
-

Seveny Fuchu
- Woonsocket, RI
- Died:
- Age: 35
- Read the obituary
-
Nydia Nayeli Sanchez
- Ft. Worth, TX
- Died:
- Age: 29
- Read the obituary
-
Cassie Phyllis Davis Miskin
- Lehi, UT
- Died:
- Age: 30
- Read the obituary
-

Savannah Blaine Settle
- Elkin, NC
- Died:
- Age: 18
- Read the obituary
-

Derline Derilus
- Boynton Beach, FL
- Died:
- Age: 33
- Read the obituary
-
Carey Morishige-Martinez
- Kaneohe, HI
- Died:
-
Wendy Rodriguez
- Pittsburg, CA
- Died:
- Age: 22
-
Amanda Lynn Wilkinson Lowery
- Eastman, GA
- Died:
- Age: 36
- Read the obituary
-

Ivelisse Pérez (Ivy) Vargas
- Perth Amboy, NJ
- Died:
- Age: 39
- Read the obituary
-

Stephanie Macias
- Las Vegas, NV
- Died:
- Age: 24
-

Joonyper Light
- Springfield, MO
- Died:
- Age: 21
- Read her story
-

Felicia Jane Sageser
- Greensburg, IN
- Died:
- Age: 25
- Read the obituary
-
Sandra Lopez
- San Diego, CA
- Died:
-
Marie Riley Sipes
- Fort Mill, SC
- Died:
- Age: 36
- Read the obituary
-
Kamilah Thompson
- Miami, FL
- Died:
- Age: 37
- Read the obituary
-

Mindy Sloan Velasquez
- Johnson City, TN
- Died:
- Age: 35
- Read the obituary
-

Christen Grace Vogel
- Jacksonville, NC
- Died:
- Age: 21
- Read the obituary
- Read her story
-
Ivy Nicole Gernhard
- Middleburg, FL
- Died:
- Age: 33
- Read the obituary
-
Tabatha Baxley
- Milton, FL
- Died:
- Age: 29
- Read the obituary
-
Rory Nunley
- Allen, TX
- Died:
- Age: 43
- Read the obituary
-
Kalayla Baert
- Wasilla, AK
- Died:
-
Courdeja Keshaune (Deja) West
- Charlottesville, VA
- Died:
- Age: 18
- Read the obituary
-
Christina Randell Penrose-Willis
- Glendale, AZ
- Died:
- Age: 35
- Read the obituary
-
Marla Anne Wingate
- Pataskala, OH
- Died:
- Age: 35
- Read the obituary
-
Catherine Gaskins
- Muncie, IN
- Died:
- Age: 37
- Read the obituary
-
Tricia Joy Drake Pless
- Elberton, GA
- Died:
- Age: 37
- Read the obituary
-
Jennifer Mae Lanning
- McKinney, TX
- Died:
- Age: 39
- Read the obituary
-
Susan Gacheri Eldad
- Atlanta, GA
- Died:
- Age: 39
- Read the obituary


Comments powered by Disqus