ProPublica is a nonprofit newsroom that investigates abuses of power. Sign up to receive our biggest stories as soon as they’re published.
The beaches of the Jersey Shore are set to reopen on Friday. But in a state where nearly 11,000 people have been killed by COVID-19, the same public health system that struggled to implement widespread testing faces what could be an even larger challenge: preventing a second wave of infection that experts say is almost inevitable without coordinated, aggressive efforts.
And more than almost any state in the country, New Jersey relies on small, local health departments, which have found themselves stretched far beyond their missions by the pandemic.
In Kearny, a town of 41,000 where the coronavirus has killed more people than in eight states, the Health Department has four full-time workers. Before the pandemic, one of them, Kristine Schweitzer Budney, was responsible for dog vaccinations, tattoo parlor licensing and restaurant safety plans.
Now Budney runs the town’s contact tracing efforts, and on top of that, she is expected to closely monitor nursing homes as they implement new infection controls.
The town of Princeton had one of the state’s first “superspreading events,” a dinner party in February that would be linked to at least 15 infections. When Dr. George DiFerdinando Jr., chair of the town’s Board of Health, contacted the state for help investigating the incident, he said he was told the town was on its own. There may have been far more than 15 cases, he told ProPublica, but “without state coordination, we couldn’t get a final number.”
The structure of New Jersey’s public health system, which is made up of roughly 100 local agencies, along with the state Department of Health, has left some cities dependent on personal connections and good fortune to secure critical resources during the pandemic. The state, with 9 million residents, has far more local health departments than California or Texas. In New Jersey, some departments cover small towns and have as few as two full-time workers. Others span an entire county and have as many as 75 employees.
Like no crisis in the state’s history, the pandemic has highlighted the limitations of the patchwork system and the challenges of coordinating a response among such a disparate array of agencies.
Many of those local departments used to receive dedicated state funding. But in 2010, in the aftermath of the last recession, that state support was eliminated. Over the last decade that has meant the loss of tens of millions of dollars for the often modest budgets of local health departments.
Per capita, New Jersey ranks 31st in the nation in state funding for public health, according to a recent report by the nonprofit Trust for America’s Health, and it ranks last in grant funding from the Centers for Disease Control and Prevention.
“Public health has been cut to the bone, and because of that, when you are faced with the pandemic, or any kind of epidemic, you know that you do not have all the staff that you need to fight it the way that you should,” said Paschal Nwako, the health officer in Camden County in the southwest part of the state, just outside Philadelphia. “We should have been prepared for this kind of public health pandemic. We prepare for emergencies. We go through training, but still, we are underfunded.”
When the pandemic hit New Jersey in March, the state health agency’s top public health job was vacant, and more than two months later, the agency is still working to hire a permanent appointee. In the interim, the job’s responsibilities have been given to the state’s chief medical examiner.
ProPublica spoke with over 30 local health directors, municipal officials and health care leaders across the state, and many of them say that in responding to the pandemic, they’ve had to carry out critical tasks, like rolling out testing and securing personal protective equipment, with little guidance or support from the state.
In some of the communities covered by smaller departments, secretaries and recreation workers have been enlisted to follow up with people who were tested, provide test results, and in positive cases, conduct contact tracing to identify and alert anyone who was connected to the infected person.
And as COVID-19 deaths in New Jersey nursing homes were mounting last month, the state delegated oversight of outbreaks in the facilities to local health agencies, saddling them with a responsibility that several said they were ill-prepared to handle.
The state has defended its response to the pandemic, and some local officials have praised the Health Department’s leadership, including Commissioner Judith Persichilli, who, along with Gov. Phil Murphy, has presided over daily briefings in Trenton, the state capital.
Other states, including Massachusetts and Pennsylvania, took a more centralized approach to contact tracing, with the states taking the lead and sharing the work with local departments. By contrast, New Jersey’s effort has been “largely a regional or local” one, said Nancy Kearney, a state Health Department spokeswoman.
Last week, as Murphy faced questions about the need to expand testing so restrictions could be relaxed for reopening, the state announced a partnership with the School of Public Health at Rutgers University to bring in more contact tracers and increase testing.
Even as New Jersey bolsters its efforts to contain the disease, officials are also beginning to scrutinize the state’s early handling of the outbreak, particularly the calamitous toll of COVID-19 on nursing homes across the state. Residents and employees in long-term care facilities account for roughly 40% of all New Jersey’s COVID deaths that have been confirmed by a lab. According to state reports, there have been outbreaks in over 500 facilities, with more than 28,000 people infected and at least 4,000 dead. This month, the Murphy administration hired a team of outside experts to evaluate the state’s nursing home regulations and oversight mechanisms.
Many local health departments have questions of their own about how the state responded to the surge in deaths in nursing homes, and in particular the surprise directive to local health departments on April 22 that they would be the primary point of contact for infection control at and inspection of long-term care facilities.
DiFerdinando of Princeton said his Health Department was blindsided by the order and didn’t have the experience or legal authority to effectively oversee the three facilities in his town, two of which have active outbreaks.
“But by this memo, you are responsible for making sure the nursing homes in your area are following guidelines,” he told ProPublica.
Dr. David Barile, medical director of the Princeton Care Center nursing home, said that when his workers started getting sick, he reached out to the local Health Department for help with staffing and acquiring protective equipment.
Barile initially told ProPublica that he did not receive PPE from the Princeton Health Department, but after this story was published, he said that he misspoke and did receive 50 gowns from the department. He also sent staff to the local hardware store to buy painter jumpsuits and masks. And in the end, 18 of his 110 residents died from the virus or related complications.
Barile called the decision to task the local Health Department with overseeing nursing homes “asinine.”
Asked about such concerns, Donna Leusner, a state Health Department spokeswoman, cited the directive, saying that the state “provides guidance on surveillance and reporting and infection control,” but local departments are “required to work with the facility to ensure these recommendations are implemented” and to investigate outbreaks.
For weeks, as thousands died in New Jersey’s nursing homes, Barile wrote letters to the governor pleading for Murphy to send in the National Guard to help overwhelmed nursing homes. In one open letter on May 1, he described facilities using trash bags and raincoats as personal protective equipment. “As of today,” Barile wrote, “all you have done for our sickest, most frail population is to loosen requirements and turn on the lights so everyone can watch as cases climb, and more people die.”
The next day, a reporter asked Murphy about Barile’s letter, and within a week Murphy announced he was deploying Guard members to long-term care facilities.
This month, the state has directed nursing homes to have all staff and residents tested. But when the state had tried to get nursing home residents tested in Kearny, it did not go as planned.
On May 4, state officials informed Budney that they would be sending supplies to Kearny’s nursing homes so that they could test all residents. But when the tests arrived, there weren’t nearly enough to test everyone, she said, and some of the kits were broken or missing swabs. They also came without instructions. Budney has repeatedly called various state offices to ask for guidance, but she said that after more than a week, she’s been unable to get an answer.
Budney is troubled by the oversight duties that have fallen on her shoulders. “I don’t think I should ever have been responsible for oversight of the care facilities in that way,” she told ProPublica. “Because I didn’t have any training.”
The early weeks of the crisis in particular were marked by a lack of communication from the state, Kearny’s mayor, Alberto Santos, said. “We felt that we were on our own. It felt like I’d woken up in this Hobbesian world where there’s no structure and everyone had to figure it out for themselves.”
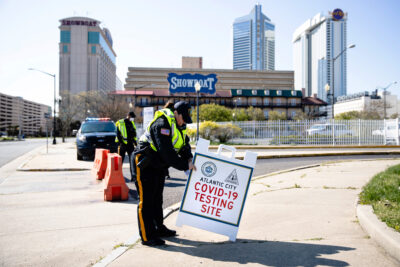
For critical tasks like testing and securing PPE for first responders, Kearny was left to its own devices. To get testing for all of Kearny’s residents, including the uninsured, Santos had to personally contact a corporate lab CEO.
Budney has experience investigating outbreaks like Legionella and food poisoning, but nothing of this magnitude. While she said that the state has been “incredibly supportive” with medical questions, for contact tracing, she’s spent many hours tackling bureaucratic hurdles on her own. For instance, she said that frequently, when a lab tells Kearny a patient tested positive, the lab won’t provide a phone number or address for the patient.
Some New Jersey agencies use commercial databases to track down phone numbers, and Budney has been trying to get access to one for nearly a month. Weeks after signing a contract, however, she’s still making calls to the company to be approved for access. Until then, Kearny’s contact tracers have no way to track down many of the people who have tested positive.
Many health department employees told ProPublica they were concerned that as the state reopens, the demands on their time will increase, as they have to resume normal work, like restaurant and beach inspections, while continuing to contact trace if cases spike. (Leusner said as much, in noting that local health workers who “may have been helping with contact tracing have to inspect community pools for reopening this weekend.”)
In recent days, the state has been marshaling additional resources for local health agencies. It is preparing to send 10 retired health officers to assist some of the local agencies, and it is also developing the more centralized contact tracing workforce with Rutgers. Leusner further said the state has awarded $5 million in federal emergency funds this week to the nonprofit New Jersey Association of County and City Health Officials to distribute to local departments. The state also brought in McKinsey, a corporate consulting firm, to advise on “public health infrastructure work, modeling and long-term care issues.”
Since the state funding was cut in 2010, many departments have had to reduce staffing, said John Saccenti, executive vice president of the New Jersey Local Boards of Health Association and a past president of the national organization for local health boards.
When Saccenti became involved in the national group, he saw how much local health funding varies from state to state: “I thought everyone was like New Jersey. And then I realized, ‘Oh my God, the rest of them are functional.’”
Last year, New Jersey’s Health Department announced it would send $2.3 million to local health departments for work on communicable diseases. Unlike the old funding structure, jurisdictions had to compete for grants and the money ended up going primarily to larger county departments, not smaller municipal ones.
“We haven’t up until now acknowledged that we should be giving to public health,” said state Sen. Joseph Vitale, chair of the senate’s health committee. “Without a thoughtful public health dynamic in our state, we set ourselves up for failure.”
While other hard-hit states significantly increased their testing over the last two months, New Jersey’s numbers remained relatively constant. In daily press conferences, Murphy periodically described plans to expand testing, but New Jersey actually reported more tests in the first week of April than it did in the first week of May.
Last week, New Jersey’s testing numbers increased substantially, though that came after the state changed its reporting to include more small labs.
In Hudson County, the choice to place the first testing center in the 20,000-person town of Secaucus created issues for the much more populous Jersey City. The Secaucus site was drive-thru only, which made it inaccessible for many Jersey City residents without cars. This concern was echoed by officials across the state, who told ProPublica that the state’s early emphasis on drive-thru testing created significant barriers, particularly for low-income communities.
Jersey City eventually set up testing on its own, but the city’s mayor, Steven Fulop, said the state has far more resources to deal with the pandemic.
“Absent a coordinated response from the top, municipalities have no choice,” Fulop said. “We’re doing it with glue and Scotch tape and duct tape and paper clips.”
In southern New Jersey, Camden County’s health officer, Nwako, said Camden was on its own, too. But with a single health agency servicing all 37 municipalities, he and his team of 75 workers were in a better position to battle the virus as it spread south.
“We have been doing the testing on our own,” he said. “We did not have any kind of help from the state, and I get it.” The state was tied up with outbreaks in the north, and every area was trying to adapt to the new demands of the pandemic, Nwako said. But the obligations just kept piling up.
“It was a total shock for me when I heard from the state that it was my responsibility to go into the long-term care facilities,” he said. “They didn’t call it an inspection, because technically we aren’t going in there to inspect.”
Perry Halkitis, dean of the Rutgers School of Public Health, said he has been deploying student volunteers to assist some local departments, but the fragmented public health structure has made his efforts more complicated and time-consuming.
“My challenge with the whole department of health situation in New Jersey is that there is not one central department of health leading the way,” he said.
Santos, the mayor of Kearny, said that New Jersey’s system of small health departments was built for things like geese control and periodic counts of all the dogs in the area (which was required by law until 2015).
“It seems to me that the person doing the dog census and the person fighting the worst crisis of our time should be different,” Santos told ProPublica. “That whole model needs to be rethought.”
Update, May 22, 2020: This story was updated to reflect that Dr. David Barile, medical director of the Princeton Care Center nursing home, received gowns from the Princeton Health Department. Initially he said he received no assistance, but after publication of this story he said he misspoke.
Filed under: